PSP is measured exclusively on the abioSCOPE
Sepsis is a time-sensitive emergency and according to the Sepsis Alliance, 80% of sepsis-related deaths could be prevented, but it remains notoriously difficult to diagnose due to the non-specific nature of its symptoms, which often resemble those of other common conditions. Timely detection and intervention are critical, as delayed antibiotic therapy in septic shock increases mortality by 8% per hour1. The current Sepsis-3 definition emphasizes organ dysfunction measured by SOFA score2. However, sepsis symptoms are nonspecific, complicating early diagnosis3.
1 (Ventura et al., 2023), 2 (Singer et al., 2016), 3 (Fidalgo et al., 2022)
Reveal Sepsis Up to 72h Before Clinical Recognition
How does Pancreatic Stone Protein improve patient care?

Pancreatic Stone Protein (PSP) has emerged as a promising biomarker for sepsis diagnosis and outcome prediction4. PSP, secreted by the pancreas, plays a crucial role in the neutrophil response during sepsis5.
PSP runs exclusively on the abioSCOPE®, an award-winning rapid diagnostics platform that leverages nanofluidics to deliver lab-quality results from a drop of blood in 7 minutes. Seamlessly integrated into routine clinical workflows, the test delivers fast, accurate, and user-friendly results in critical care settings. By measuring PSP levels, which are directly linked to a patient’s risk of sepsis, the test enables healthcare professionals to activate sepsis bundles earlier and improve outcomes.
4 (Zuercher et al., 2023; Fidalgo et al., 2022), 5 (Eggimann et al., 2019)
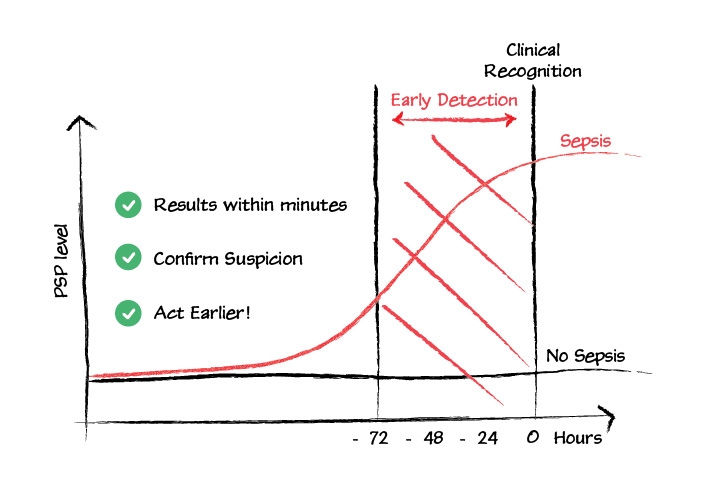
PSP levels increase earlier in the infection process than traditional biomarkers, offering the potential for earlier sepsis detection. Research shows that PSP levels can rise up to 3 days before clinical diagnosis6. This early detection is especially beneficial in EDs, where PSP aids in early diagnosis, reducing unnecessary antibiotic use and supporting stewardship strategies7. Its diagnostic potential has been validated in emergency departments (EDs) and intensive care units (ICUs)8.
PSP also serves as a reliable prognostic marker for ICU mortality, outperforming CRP and matching PCT in predictive power9. Its use in assessing severity and predicting mortality in septic patients allows for better resource allocation and patient stabilization.
A key advantage of PSP is the availability of near-patient tests, which enable rapid, cost-effective bedside measurements within minutes10. This quick turnaround is vital in high-stakes environments such as ED and ICU.
6 (Pugin et al., 2021), 7 (Fidalgo et al., 2022), 8 (Prazak et al., 2021), 9 (Zuercher et al., 2023), 10 (Schneider et al., 2022)
Testimonials
Advantages
EARLIER DETECTION OF SEPSIS
PSP level rises up to 3 days before clinical recognition enabling faster intervention and improved outcomes.
RELIABLE PROGNOSTIC VALUE
Higher performances to current Standard of Care in predicting ICU mortality, enabling clinicians to better evaluate disease severity.
RAPID NEAR PATIENT TESTING
PSP is exclusively measured on the abioSCOPE® platform, delivering lab-quality results within minutes from a drop of blood.